-
Posts
926 -
Joined
-
Last visited
Content Type
Profiles
Forums
Events
Posts posted by Function
-
-
If I recall correctly, UPS is indeed involved in it (and disturbed); there are many factors causing PD; Lewy bodies are aggregations of synuclein-alpha proteins, try to look a bit further into that matter too
if I have any time these days (very short on time now), I might try to look up the pathogenesis of PD again in my neurophysiology course slides .. due when is your essay?
0 -
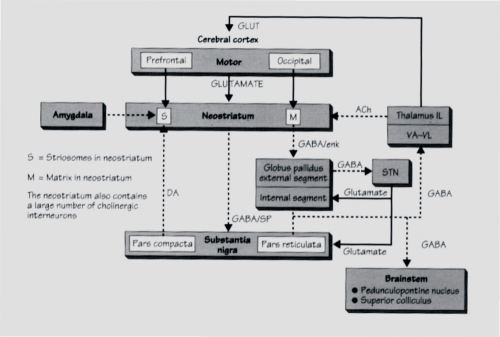
A picture says more than 1000 words .. Are you familiar with the basal ganglia and their effects on one another? It may be very interesting to draw a scheme displaying effects (excitatory vs. inhibitory) of:
- Amygdala
- Neostriatum: striosomes & matrix
- Substantia nigra
- Compact part
- Reticular part
- Globus pallidus, external part
- Globus pallidus, internal part
- Subthalamic nucleus of Luys
- Ventral anterior and ventral lateral nuclei of thalamus
- Intralaminar nuclei of thalamus
- Prefrontal cortex, primary motor cx, parietotemporal cx
- (Optionally, superior colliculus and pedunculopontine nuclei)
on one another. We saw such a scheme and I memorised it and can still reproduce it. It is then very handy to distinguish a direct pathway from an indirect pathway in the basal ganglia (look it up), and the role of D1 and D2 dopamine receptors in these pathways, consequently describing the effects of dopamine on these pathways and, eventually, excess/deprivation of dopamine.
This is the scheme we were supplied by our neuroanatomy professor. Try to distinguish the direct from indirect pathway (look it up) and role of D1 and D2 and where things go wrong in HD and PD.
0 -
"In Paradisum", part VII of the Requiem in d minor, Op. 48, by Gabriel Fauré - rendition by P. Herreweghe
And "Broken Crown" by Mumford & Sons
0 -
Hello everyone
In order to write a paper, I need to understand the "precursor-product model" formula in order to calculate the FSR of mixed muscle protein.
In articles using marked phenylalanine as a tracer, this is the given formula
[math]FSR=\frac{\Delta E_p}{t} / \left[\frac{E_{M1}+E_{M2}}{2}\right]\cdot 60\cdot 100[/math]
Where Delta(Ep) would be the increment in protein bound tracer, and EM1 and EM2 being "the phenylalanine enrichments in the free intracellular pool in the 2 sequential biopsies" and t being the time.
I've got 2 questions:
- Can someone clearly explain to me EM1 and EM2, and why one should divide Delta(Ep) by the mean of EM1 and EM2?
- Why does one multiply by 60?
In articles using marked leucine as a tracer, this is the given formula
[math]FSR=\frac{\Delta L_m}{L_p}\cdot\frac{1}{t}\cdot 100[/math]
Delta(Lm) is similar to Delta(Ep) and Lp would be "the mean value over time of venous alpha-KIC labelling" and t again the time.
Can someone, in accordance to my questions above, explain to me Lp and why one divides by this Lp? And why no factor similar to 60 here?
Thanks!
Function
0 -
You may understand that in order to reduce mean pressure (MABP), you may have to dilate your vessels. By extension, you may appreciate that vessels with a larger diameter possess less resistance. Ta-da.
Another phenomenon you might be interested in, is the windkessel effect (look it up on Wiki), it's a phenomenon describing why blood pressure doesn't fall to 0 mm Hg after systole, but drops to and remains at about 80 mm Hg until the next systole
1 -
It may be interesting to appreciate that every rib, with exception from the 1st, 11th and 12th, articulate with 2 vertebrae using 3 articulations:
- Rib X (not 10th, just a random rib) will have articulations with
- Vertebra X-1, more specifically the inferior articular pit by the uppermost articular face on the head of the rib (caput costae), divided from the lowermost by the crest of the head of the rib (crista capitis costae)
- Body of vertebra X, more specifically the superior articular pit, by the lowermost articular face on the head of the rib; although there are, in fact, 2 articular faces on a head of a rib, we, in osteology, only describe 1 "facies articularis capitis costae" (articular face of the head of the rib)
- Transverse process (proc. transersus) of vertebra X, by the articular face (facies articularis tuberculi costae) on the costal tubercle (tuberculum costalis)
0 - Rib X (not 10th, just a random rib) will have articulations with
-
Xalatan is most likely right. Most likely because we're dealing with very fragile, mostly unexplored matters here. I'm afraid I stopped reading KMC's reaction right when I read that memories are stored in the hippocampus. It has been shown (I have no source but you'll have to accept from me that it was mentioned in my neurophysiology syllabus 2015), that memories are indeed 'stored' in places relevant to the senses forming the experience evoked by the memory. For example, if you see a green cup, then chances are likely that the next day, when you see a green cup, you'll remember having seen that (or another, doesn't really matter) green cup the day before. This will have to do with synaptic plasticity (look up Hebbian synapse) mostly in the visual cortices. It is undebatable that, indeed, the hippocampus is essential in forming memories (short term and long term)
It is shown that if certain parts of the brain are stimulated, one experiences something that he or she has experienced before - a memory is begin evoked. There's also a possibility of evoking something that the patient genuinely experiences as a memory (something experienced before), but actually has not experienced in the past. Very interesting matter.
We cannot read memories. We can read thoughts, to a certain degree, however. I think that the synaptic strength (cf. synaptic plasticity, look up Hebbian synapse) between neurons firing during these thoughts make us 'remember' something, or, if not so strong, experience it for the first time. Look up the work of Belgian professor Steven Laureys who uses fMRI etc. to read his patients' minds (to a certain, limited degree!!) by giving significance to the results of the scans.
You may want to look up the video "memories are made of this" on YouTube, in which Eric Kandel, PhD (Nobel Prize, 2000, for his work about sensitization in aplysia) explains how sensitization and different types of memory work. This is of course a very simplistic circuit, but may give us an idea about how things may work in our brains.
0 -
The phenomenon Xalatan is talking about is called "suppression scotoma", it generally is the neglecting by the brain of visual input from the affected eye (be it an eye showing strabismus, or perhaps amblyopia ex anopsia ['lazy eye']), if the healthy eye (you can appreciate that if the healthy eye is covered, of course your brain will not start neglecting visual input from the affected eye) is not covered by an eyepatch during the 'critical period' of development of cortical plasticity
0 -
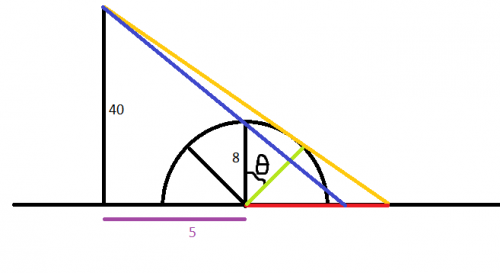
90°? Did I wrongly interpret the problem?
(red = shadow; black = pole and plate (circle because of different angles, at least this is what I interpreted), yellow the light beam between post and plate when it's placed at about 45°, blue if it's placed at 0° with the vertical)
I didn't calculate it, but shouldn't it be 45°?
0 -
Thanks, doctor
0 -
Very well ... Anyway, if the question should appear on the exam, and the answer would've been a parasympathicolytic, then there is enough evidence arguing that a sympathicomimetic would be better (even in the Commented Drugs Repertory 2014 (and perhaps also 2015, don't know; I'll receive the 2016 version next term), the book in which about every drug that can be used as therapy is listed, a book every Belgian doctor has in his lab coat or in his desk, only sympathicomimetics are listed under "nasal vasoconstrictors") and as per result, enough evidence to have the question removed
0 -
Note that the vascular smooth muscles in nasal mucosa, spongious tissue and salivatory glands (especially parotis gland) are controlled by both SNS and PSNS (they form exceptions), which is why a PSNS-antagonist does indeed relieve nasal congestion (although I don't know why one doesn't give a PSNS-antagonist such as atropine, perhaps because of the unwanted side effects on the heart rate?)
Indeed, I think that RR is the differentiating factor here; both PSNS-block (via ACh on muscarinic receptors via Edinger Westphal nucleus and oculomotor nerve) and SNS (via the superior cervical ganglion) may induce mydriasis, seen in oculomotor palsy and Horner's syndrome
0 -
A question that was asked on a previous edition of the exam concerning the cardiovascular system, was:
Nose decongestion, hypertension and mydriasis may be evoked by a
- Parasympatholytic
- Sympathomimetic
- Parasympathomimetic
- Sympatholytic
Of course, the last 2 are false.
Now, there is a big discussion on which of the 2 remaining would be the correct answer.
I plead for the sympathomimetic, whereas others prefer the parasympatholytic.
Arguments for parasympatholytic:
- Removal of the sympathetic inhibition by the parasympathetic nervous system
- Inhibition of the parasympathetic effects by the vagus nerves on SA and AV nodes, increasing heart rate
Arguments for sympathomimetic:
- Activation of myocard, smooth muscle cells in coronary arteries and also the SA and AV nodes
- Peripheral vasoconstriction (alpha-1) which, as far as I'm aware of, can not be evoked by blocking parasympathetic NS?
- Activation of the renine-angiotensin-aldosteron system by activation of renal beta-1 receptors
I think that, mainly because of the last 2 reasons, a sympathomimetic would be more useful to evoke hypertension.
Thoughts?
0 -
Please review my last comment: the easy repolarization would not be because of greater efflux, in hyperkalemia, and that is quite logic, but I think because of the ease of hyperpolarization since Na channels are already closed; might need some feedback on this one from someone with a more fundamental knowledge of the heart electricity.
Speaking of RAAS, I've developed a huge aversion for the renal physiology in the last few months since it was given to us
 I've never been a huge fan of metabolism, truth be told
I've never been a huge fan of metabolism, truth be told 
If I may, I'd suggest you to buy Ganong's Review of Medical Physiology (most recent ed.), it is the book our professors refer to in their courses and notes (of course, the paper courses by our professors form the main thing, we use handbooks if we don't understand something), and these things are, as far as I'm aware of, very well explained in it.
Should you show more interest in the CNS, my professor strongly advised me, and thus I did, to buy "Principles of Neural Science" by Eric Kandel (Nobel Prize, 2000) et al. (5th ed.); it gives you a very profound explanation on the understanding of the CNS, slightly more applied to the physiological aspect of it
0 -
Indeed, I see that hyperkalemia generally leads to activation + inactivation of VG Na-channels; you may appreciate the structure of Na-channels, comprising of an M-gate, and an H-gate; the M-gate opening very quickly at certain treshold depolarization (treshold of opening = -65 mV), and the H-gate closing very slowly, closing increasingly with depolarization; the depolarization of the membranes by K may be so fast, I think, that the time between opening the M-gate, and closing the H-gate, becomes insignificantly small. Hyperkalemia thus slows down the action potentials.
Note that in general, hyperkalemia results in arrhythmias by, as mentioned before, depolarizing the membrane, but that it slows down and weakens depolarization during those arrhythmic action potentials (which results in a decreased P-wave in the ECG, meaning a much weaker atrial depolarization), and that it significantly enhances the repolarization (T-wave) because the relative ease it gets from the closed Na channels, at the end of the action potential, which in turn gives calcium less chance to build up and cause the 'plateau' (ST-segment) of the action potential, during which the muscle cells contract.
In conclusion: hyperkalemia (1) causes arrhythmias by overall depolarization of the cell membranes, (2) slows down and weakens depolarization during action potentials, (3) enhances repolarization at the end of the contraction and (4) shortens the contraction
Fun facts: a plasmic kalemia of +5,5 mM will give you these arrhythmias; a kalemia of +8 mM will cause a heart block (not necessarily an arrest, but an arrest of the conduction at certain conductive tissues; cause will probably be the complete inactivation of all Na channels)
--
Thank you for the luck - I'm not so sure I'll fly through it, but rather hobble through it
 my interests in the cardiovascular system are by far not as great as my interests in the central nervous system, of which the exam was (strangely enough for a lot of students) - nice.
my interests in the cardiovascular system are by far not as great as my interests in the central nervous system, of which the exam was (strangely enough for a lot of students) - nice.The taste testing question did not come up
 Might've been a too ambiguous question to be posed on an MCQ exam (all our exams are MCQ, sadly enough)0
Might've been a too ambiguous question to be posed on an MCQ exam (all our exams are MCQ, sadly enough)0 -
Aye, I did understand the concept already, but thank you anyway for your answer! It might be enlightening to other users too!
Would be a huge problem if I wouldn't understand this by now, since we're taking on the cardiovascular system, respiration, kidneys and urinary tracts in 10 days; and understanding the fundamentals of electrical systems is quite necessary for this ^^
0 -
Here's what I think, based on what I know from functional neuroanatomy and neurophysiology
I think, indeed, the accommodation reflex will be preserved. So the ciliary muscle will contract (together with the sphincter pupillae muscle), being innervated by the general visceral efferent fibres in the third cranial nerve, originating the Edinger-Westphal nucleus. This, I think, is in turn connected to vestibular nuclei, which are ipsilaterally innervated by the fastigial nucleus in the cerebellum. This, in turn, receives input from the contralateral pontine nuclei, connected directly to the middle superior temporal area and indirectly to the middle temporal area (projecting into the middle superior temporal area), forming essential area's on the magnocellular pathway (important visual area's being namely V5 and V3), important for the perception and tracking of moving objects located in the contralateral visual field.
So, in short, if your left eye spots something that is coming closer, it will trigger pathways on the contralateral occipital and temporal lobes (decussation via optic chiasm), in turn triggering pathways on, again, the ipsilateral side of the left eye (decussation of pontine nuclei to cerebellum), initiating accommodation.
Just try it yourself: close your one eye and bring your finger back and forth: you'll see that it's as sharp as with both your eyes open.
I think, but this might be wishful thinking, that indeed it takes me a bit longer to accommodate than with both eyes open.
There is also a phenomenon called perceptual steadfastness, namely: you don't care if an object is black on white, or white on black, you recognize it. You don't care if an object is 2 cm away from your eye or standing 2 metres away from you, in the first case you won't think that it's suddenly a hundred times bigger. And so on.
0 -
No idea why it does specifically exit the brain stem dorsally, but a small correction (very small): your title gives the impression that it decussates after leaving the brain stem. Note that its fibres already decussate in the brain stem
0 -
If I'm not mistaken, there are several olfactory pathways that do run through the thalamus, to reach the orbitofrontal cortex. This last one is part of the neocortex, the most recent type of cortical structure in evolution, very typical for higher animal orders.
Here are the pathways I know from physiology:
- Anterior olfactory nucleus --> bilateral feedback to the olfactory tracts through the anterior commissure
- Olfactory tubercle --> thalamus --> orbitofrontal cortex | prefrontal cortex
- Amygdala --> hypothalamus, to induce feeding urge
- Piriform cortex --> thalamus --> orbitofrontal cortex | prefrontal cortex
- Entorhinal cortex --> hippocampal formation to form olfactory memory of the percepted smell
With piriform cortex being important for the true sensation of smell, and the olfactory tubercle important for emotional correlations with smell.
The other area's, as you can see, do not necessarily project through the thalamus. This is because the effects they induce are, as mentioned by the other users above, evolutionary conserved.
As far as I'm aware of, indeed, these tracts do not necessarily project through the thalamus and, in extenstion, the orbitofrontal cortex of the prefrontal cortex, but they might.
But I'm not aware of tracts leaving the piriform Cx and olfactory tubercle bypassing the thalamus.
-F.
1 -
My best guess would be that it's already occupied by the maxillary nerve (V2 < N. V, trigeminal nerve), since the round foramen itself isn't very large, I think. Exceptional is the jugular foramen, which holds passage for IX, X and XI, but that one's not very small so that doesn't form a genuine problem.
0 -
Hello everyone
Soon I'll be taking exam on the CNS. In preparation for this exam, there are multiple example questions, which were frequently asked on previous editions of the exams. They are reconstructed by fellow students of older years, who already took the exam.
One of these questions is:
Testing the gustatory sense is useful in patients presenting with:
- Dysarthria
- Diplopia
- Loss of hearing
- Hemifacial paralysis
I think 3 of these answers could be correct:
- Dysarthria because speaking involves several cranial nerves, of which Nn. VII, IX, X and XII. Of these, VII, IX and X are important for gustatory sense (VII anterior 2/3 tongue; IX posterior 1/3 tongue; X uvula), so in this case I think testing the gustatory sense might help the physician distinguish the affected nerve.
- Hearing loss because the intermediofacial nerve runs through the petrous part of the temporal bone, along with the eighth cranial nerve, the vestibulocochlear nerve. I think any space taking mass (tumor, e.g. vestibular schwannoma) might compress both nerves, inducing hearing loss, loss of taste and also hemifacial paralysis (of type Bell's palsy)
- Hemifacial paralysis; facial muscles innervated by N. VII; I think that it is indeed useful to test the taste in patients presenting with full hemifacial paralysis, both upper and lower facial muscles (in order to determine at what level the lesion might have occured: before or after the splitting of the chorda tympani?); yet not so useful in patients presenting with paralysis of only lower facial paralysis, for this would already imply a higher order lesion than a peripheral N. VII Bell's palsy.
It may be that the question was reconstructed with errors.
However, should someone be able to give me an unambiguously answer, thank you very much.
F
0 -
Exam is on 11 January ^^ The neuroradiological part is rather small and relatively - very easy
 For you the same! Happy holidays!0
For you the same! Happy holidays!0 -
Thank you for your answer. Indeed, it is most probably the left LGN.
I kind of misunderstood him, interpreting that it could not be found on the scans given to us.
The message I misunderstood he tried to spread was that they failed to outline the LGN (they forgot it or whatever), so it could not be highlighted in the program we're using to see these scans, nor could it be found in the index with structures which can be highlighted

My apologies!
0 -
You wouldn't surprise me if you told me you're going to take exam in 2 weeks
 students in the first year in medicine in our university are, and these are questions they frequently ask us... Which is why I'm answering these questions so thoroughly. Well ... that, and because I can answer them. If you happen to be a student from Ghent, forgive me for giving the anatomical terms in English, but I expect it to be no problem for you to translate them into Latin. If you're not, forgive me this small introduction, being completely irrelevant to you.
students in the first year in medicine in our university are, and these are questions they frequently ask us... Which is why I'm answering these questions so thoroughly. Well ... that, and because I can answer them. If you happen to be a student from Ghent, forgive me for giving the anatomical terms in English, but I expect it to be no problem for you to translate them into Latin. If you're not, forgive me this small introduction, being completely irrelevant to you.Now let me return on-topic and answer your questions:
(1) The mamillary and accessory processes are indeed very typical for the lumbar vertebrae, but also happen to appear on the twelfth thoracic vertebra. Under no normal circumstances are they found in cervical and other thoracic vertebrae.
(2) Being an undergraduate teaching assistant in anatomy (mostly osteology), let me give you an overview of typical structures per vertebra, with which you can easily distinguish the types of vertebrae from one another:
- Cervical
- Transverse process possess 2 tubercles and seems 'split': an anterior tubercle (NB called the carotid tubercle in C6) and a posterior tubercle, divided by a groove for the spinal nerve (sulcus nervi spinalis)
- Transverse foramen in the transverse processes (for passage of both vertebral arteries)
- Split spinous process
- Upstanding lateral ridges of the vertebral body, called the uncinate processes
- Thoracic
- Superior and inferior (excl. T12) costal pit
- Costal pit of the transverse process (excl. T11, T12)
- Sharp, unsplit spinous process
- Lumbar
- Very obvious, stumpy, almost rectangular spinous process
- No superior, nor inferior costal pit
- No costal pit on the transverse process, which is here called a costal process
- Very broad vertebral body
- Mammillary and accessory processes
It may be a challenge to distinguish a random lumbar vertebra from the twelfth thoracic vertebra. To distinguish them from one another, you must keep in mind that the twelfth thoracic vertebra stil possesses a superior costal pit, yet no inferior pit, nor a costal pit of the transverse process (which also isn't found on the eleventh thoracic vertebra, btw, since the eleventh and twelfth ribs (the floating ribs, costae fluctuantes) don't have a costal tubercle which can articulate with a costal pit of a transverse process).
There you go! Best of luck with the rest of your studying and perhaps even good luck with your exam.
Function
Sources: Sobotta, Atlas of Human Anatomy - General Anatomy and Musculoskeletal System (for solving my doubts on vertebra T12) & a hopefully credible experience as an undergraduate teaching assistant in anatomy (for all the other stuff)
0 - Cervical

Ashkenazi Jewish intelligence
in Psychiatry and Psychology
Posted
Looks like someone's about to reconsider his creed